|
|
|
| Prosthetic Rehabilitation Of Pediatric Patients |
Gp. Capt. Satish Kumar Gupta 1 , Wg. Cdr Shashi 2
1 Dy. Comdt., Prosthodontist - Airforce institute of Dental Sciences, Bangalore
2 Prosthodontist, Airforce Dental Centre - Delhi Cantt
|
| Address For Correspondence |
Address For Correspondence:
Gp. Capt. Satish Kumar Gupta
Dy. Comdt., Prosthodontist
Airforce institute of Dental, Bangalore
Email ID : guptasatish_27@yahoo.com
Phone : +917351588444 |
| Abstract |
| Edentulism or tooth loss is considered as a major health problem that has serious emotional, social, and psychological consequences affecting a child’s nutrition, esthetics, self-confidence and self-esteem. Common causes for edentulism in children are; dental caries, traumatic injury, congenital absence of teeth, congenital malformation of teeth, cleft lip and palate. Prosthodontic rehabilitation of children with pronounced edentulism helps to restore masticatory function, appearance and muscle function; to maintain and improve phonetics; prevent development of deleterious oral habits; and, to minimize possible psychological disturbances. Different treatment modalities for prosthetic rehabilitation in infants\children\adolescents are removable partial dentures, complete dentures, partial dentures fixed with orthodontic bands or Nance dentures, various kinds of crowns like stainless steel crowns, polycarbonate, composite strip crowns, resin bonded prosthesis, fiber reinforced fixed dental prosthesis etc. Prosthodontic treatment of children often requires highly intricate procedures with cooperation from patient and as well as from parents. |
|
| Keywords |
| Pediatric rehabilitation, Obturators, Implants, Speech prosthesis. |
|
| Full Text |
Introduction
In-spite of scientific advancement in the area of preventive dentistry, access to use of dental services, systemic and topical fluoridation, there is a substantial prevalence of edentulism in children and adolescents[1]. Edentulism or tooth loss is considered as a major health problem that has serious emotional, social, and psychological consequences affecting a child’s nutrition, esthetics, self-confidence and self-esteem.Children are often affected psychologically by the unacceptable appearance of diseased, damaged or missing teeth,one should not allowchronologic age to preclude performance of whatever treatment is necessary to provide proper function and esthetics. If teeth involved are fully erupted, have achieved complete root formation, and may be prepared without causing irreversible damage to pulp, successful prosthodontic treatment can often be provided for patient as young as 12-14 years of age. Prosthodontic treatment of children often requires highly intricate procedures with cooperation from patient and as well as from parents.
Definition Of Age Group Terminology
According to American Academy of Pediatrics Committee on Fetus and Newborn, pediatric patients are defined as follows [2] [Table 1]
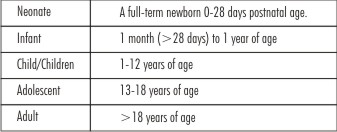 | Table 1
 |
Causes And Prevalence Of Edentulism In Children
Despite significant improvements in oral health among children, tooth loss remains a dental public health problem among adults. The most important function of dental profession is to prevent tooth loss. Common causes for edentulism in children are;dental caries (rampant and nursing bottle caries ), traumatic injury, congenital absence of teeth (partial or complete anodontia) as in case of ectodermal dysplasia, congenital malformation of teeth as in case of amelogenesis and dentinogenesis imperfect and cleft lip and palate[3].
Consequences Of Premature Tooth Loss
Premature loss of tooth can lead to loss of space in mixeddentition which in turn can lead to malalignment of teeth.Early loss of primary incisors or molars can lead to deleteriousoral habits like anterior or lateral tongue thrusting respectively. Congenital absence of anterior teeth or loss due to traumacan cause psychological trauma to children because ofunintentional, yet unkind remarks by friends or relatives. Thiscan lead to a feeling of rejection or inadequacy regarding theirpersonal appearance. Missing primary anterior teeth can leadto temporary misarticulation of consonants in speech. Apart from this, other effects of edentulism are
Reduced masticatory efficiency
Lack of facial support and aesthetics
Loss of vertical dimension of occlusion
Loss of alveolar ridge height
Benefits Of Restoration Of Missing Teeth
Restoration of anterior teeth restores the appearance andthe self-confidence of children[4]. Many children with earlychildhood caries who had untreated carious anterior teeth will be extremely happy after full mouth rehabilitation with strip crowns or anterior stainless steel crowns. Restoration of missingposterior teeth can enhance the efficiency of mastication andanterior teeth can lead to better speech pattern. Constructionof dentures or fixed replacements of anterior teeth can preventdevelopment of deleterious oral habits. Some of the removabledentures can serve as space maintainers as well.
Examination, Diagnosis And Treatment Plan:
Prosthodontic treatment is based upon the results of a clinical examination and is ideally part of a comprehensive treatment plan. Clinical examination of the child is carried out in usual manner. Radiographic examination involves panoramic radiographs, in that one could visualize different stages of development at which the various succedaneous teeth are at that particular point of time. This information helps prosthodontist to predict approximate time and sequence of eruption of succedaneous teeth and also decide whether particular patient presents the indication for prosthesis.Treatment plan shall take into consideration[5]
1. Developmental status of the dentition;
2. Caries-risk assessment;
3. Patient’s oral hygiene;
4. Anticipated parental compliance and likelihood of recall;
5. Patient’s ability to cooperate for treatment.
The restorative treatment plan must be prepared in conjunction with an individually-tailored preventive program. Caries risk is greater for children, who are poor, rural, or minority or who have limited access to care. Factors for high caries risk include decayed/missing/filled surfaces greater than the child’s age, numerous white spot lesions, high levels of mutans streptococci, low socioeconomic status, high caries rate in siblings/parents, diet high in sugar, and/or presence of dental appliances. Studies have reported that maxillary primary anterior caries has a direct relationship with caries in primary molars, and caries in the primary dentition is highly predictive of caries occurring in the permanent dentition.
Rehabilitation Of Adults Vs Pediatric Patients:
Restoration
Restoration of primary teeth differs from restoration of permanent teeth, due to the following factors[6].
Differences in tooth morphology. The mesiodistal diameter of a primary molar crown is greater than the cervico-occlusal dimension. The buccal and lingual surfaces converge toward the occlusal surface.
The enamel and dentin are thinner.
The cervical enamel rods slope occlusally, ending abruptly at the cervix rather than being oriented gingivally and gradually becoming thinner as in permanent teeth.
The pulp chambers of primary teeth are proportionately larger and closer to the surface.
Primary teeth contact areas are broad and flattened rather than being a small distinct circular contact point, as in permanent teeth.
Shorter clinical crown heights of primary teeth also affect the ability of these teeth to adequately support and retainrestorations.
Young permanent teeth also exhibit characteristics that need to be considered in restorative procedures, such as large pulp chambers and broad contact areas that are proximal to primary teeth.
Impression Procedures: Making impression in children is challenging owing to
Lack of cooperation from child
Anxiety
Small opening of mouth
Difficulty in tray selection
Difficulty in controlling salivation
Children may be anxious about having impressions made and a careful explanation should be given before starting the procedure. Appropriate tray selection is important while making impressions. The amount of impression material taken on the tray should be just adequate to make an impression. Any excess material on the tray may be displaced into the pharynx and cause gagging. The posterior half of the tray may be loaded with less impression material. While placing the tray inside the mouth, it is positioned anteriorly and pressed against the teeth which will displace the excess impression material posteriorly to compensate for the less material in the posterior half of the tray. This technique works well with impression making in children. While making the impression, the operator should have a tongue mirror or tongue blade to remove the excess impression material from the posterior palatal area.
Distraction Techniques:
a. Asking the child to raise his or her finger or thumb as specified.For e.g. show me the right little finger or left thumb or left middle finger, etc.
b. Asking the child to lean forward and breathe through the mouth
c. A small dab of alginate is placed over the child’s thumb or finger and asked to raise the hand once it sets
d. Asking the patient to breathe rapidly
e. Asking the patient to raise the legs alternatively and point the toe towards the roof
f. Asking the patient to count within himself till 30 or 50
Different Treatment Modalities in Prosthetic Rehabilitation of Pediatric Patients:Different treatment modalities for prosthetic rehabilitation in infants\children\adolescents are as follows. [7]
1. Removable partial dentures
2. Complete dentures
3. Partial dentures fixed with orthodontic bands or Nance dentures
4. Various kinds of crowns like stainless steel crowns, polycarbonate, composite strip crowns
5. Resin bonded prosthesis
6. Fiber reinforced fixed dental prosthesis
7. Porcelain laminate veneers
8. Feeding plates in infants
9. Palatal obturators in CLP patients.
10. Speech prosthesis for velopharyngeal deficiency or velopharyngeal incompetency.
11. Osseointegrated implants.
Removable Partial Dentures:
The removable partial dentures arefairly tolerated bychildren and are commonly used successfully to prevent consequencesof premature tooth loss.[8]
Important Considerations in Design of RPD in Children:
1. Full palatal coverage for maxillary partial dentures
2. Relatively short and contoured buccal or labial flanges
3. Clasps when used around primary canines should be removed at appropriate time to allow thecuspids to drift laterally and distally to accommodate the erupting permanent incisors
4. For mandibular RPD with lingual bar, the bar should be adapted 2mm away from the soft tissue so that it will accommodate the developmental changes in the dental archwhen succedaneous teeth starts erupting
5. When necessary the RPD should be fabricated before extraction of teeth and used as immediate partial denture as well as immediate space maintainer
6. The teeth are set with spaces and in a more vertical axis than in adult dentures.
7. As the child grows it may be necessary to remove portion of the appliance to allow for eruption of permanent successors.
Complete Dentures:
Indications:
1. Children with genetic diseases in which missing teeth are a part of the syndrome often need complete dentures to restore the primary and permanent dentition. Eg: Ectodermal dysplasia with anodontia or oligodontia. [9]
Important Considerations in Fabrication:
1. Children with ectodermal dysplasia continue to exhibit normal facial growth except for alveolar bone deposition. There is a need to periodically remake the prosthesis and esthetically customize denture to the child’s current stage of dental and facial development.
2. Making a centric relation records is difficult in children because they do not have same musculature, TMJ functions or growth maturity as in adults. Unfortunately all prosthetic principles are directed towards adults. To overcome the problems zero degree teeth are arranged in flat occlusal plane.
3. Over denture may be fabricated using existing teeth for retention of the denture and preservation of alveolar bone.
Resin Bonded Metal Ceramic Fdp:
For reason of pulpal and periodontal health and conservation of tooth structure, resin boded prosthesis should be the first choice whenever possible[10]. Retention and resistance is achieved through preparation in enamel, coupled with acid etching of enamel and fixation with adhesive resin cements.
Indications:
1. Congenitally missing teeth.
2. Tooth lost due to trauma.
3. Adequate clinical crown height.
Contraindications:
1. Poor oral hygiene.
2. Large carious lesion in abutment.
3. Malpositioned teeth.
Advantages:
1. Conservation of teeth structure, reducing trauma to pulp.
2. Can be done without LA.
3. Excellent esthetics.
4. Failure can be easily repaired.
Disadvantages:
1. Cannot be given where large restoration or caries exists in abutment tooth.
2. Cannot be given in malpostioned arches, deep bite and caries prone individuals.
Fiber Reinforced Fixed Dental Prosthesis
There are situations in which a semi permanent fixed dental prosthesis may be desirable, particularly for patients who have completed orthodontic treatment but are too young to embark on implant therapy. Following advances in fiber reinforcement technology, fiber-reinforced composite resin (FRC) now represents a lower-cost alternative to traditional metal-ceramic for the construction of resin-bonded prostheses in case of children.
It has a number of potential advantages compared with a metal framework of traditional RBP. Improved adhesion of the resin luting agent to the framework, potential for improved esthetics, and physiologic stiffness of the framework material. The most commonly used FRCs consists of glass fibers embedded in a dimethacrylate resin matrix. An alternative system is based on the use of a multiphase polymer matrix of linear polymer with a dimethacrylate resin. A multiphase polymer matrix of FRC is proposed to improve adhesion between the veneering composite and composite luting agent to the FRC framework.
FDPs constructed from FRC may be retained using complete-coverage crowns, inlays, surface-retained wings, or a combination. The use of full-coverage retainers has been recommended; however, the preparations required for these are as extensive as those required for metal-ceramic reconstructions. In current clinical practice, FRC-FDPs are most commonly surface or inlay-retained to minimize the need for tooth preparation.
The preparations consist of removing approximately 1.0 mm of enamel on the palatal and proximal aspects of the abutment teeth. All gingival margins should be in enamel, chamfered and supragingival. The internal line angles should be round, and the gingival floor to be prepared with a butt joint.
The first step in the final cementation of the restoration is to etch enamel with 35% phosphoric acid gel for 20 seconds. The teeth are then rinsed and gently dried. Dentin bonding agent should be applied to the preparations following the manufacturer’s instructions followed by gentle air thinning and light curing. The FRC-FDP restorations should be slowly seated and any gross excess of cement removed. Continuous pressure should be maintained on the restoration during initial light curing, 5 seconds for each abutment.
Obturators
A palatal obturator is a prosthesis that totally occludes an opening such as an oronasal/oroantralfistula. Palatal obturatorstypically are prosthesis used to close defects of the hard/soft palate that may affect speech production or cause nasal regurgitation during feeding. Following surgery, there may remain a residual oronasal opening on the palate, alveolar ridge, or labial vestibule. A palatal obturator may be used to compensate for hypernasality and to aid in speech therapy targeting correction of compensatory articulation caused by the cleft palate. Palatal obturators are indicated in individuals with cleft palate, operated cases of surgical resection of tumors and children with traumatic injuries.[11]
Feeding plate or feeding appliance:
Cleft lip and palate are one of the most common structural birth defects. Its consequences affect several systems and functions that include feeding, facial growth, dentition, speech as well as the social and psychological problems which have an impact on the child and parents. Neonates born with cleft lip and palate have oronasal communication which diminishes the ability to create negative pressure necessary for suckling[12]. Compressing the nipple between tongue and hard palate to squeeze out the liquid becomes difficult. Feeding appliances are often required by such patients. A feeding appliance is a device that creates a seal between the oral and nasal cavities and helps the infant to express milk. Sucking efficiency is one of the most common difficulties related to feeding in children with cleft lip and palate. In order to be successful in sucking, coordination of the intraoral muscles is important, which may be difficult in children with cleft lip and palate. Breast feeding a child with a cleft palate can be challenging. The opening in the palate makes it impossible for the child to create suction. The baby may have difficulty in locating a place on the palate to press the breast against and to express milk. However, the amount of difficulty will vary based on the severity of the cleft. There are a variety of feeding devices that can be very useful in successfully feeding an infant with a cleft lip and palate, like a plastic squeeze bottle, soft nipple, specially designed nipple with enlarged opening and wide based nipple (useful in sealing off the cleft lip). A feeding obturator is a device that creates a seal between the oral and nasal cavities and controls the flow of milk. Feeding device is inserted over the infant's hard palate, which allows him or her to compress the nipple easier because it provides a contact point and helps the infant to express milk. It facilitates feeding, reduces nasal regurgitation and shortens the length of time required for feeding. Either heat cured acrylic resins or ethylene vinyl acetate can be used for the fabrication of feeding plate. Feeding appliance made with ethylene vinyl acetate has many advantages over acrylic feeding appliance, which are as follows:
1. Smoother surface
2. Soft in nature
3. No need of retentive wire
Palatal Plate is a kind of obturator, generally consisting of an acrylic plate and retention clasps of orthodontic wire, which covers a fistula of palate. It may be used to aid in improving articulation and feeding. The blockage of the opening helps to improve hypernasality and suckling ability for babies. In the case of a labial-oral-nasal fistula, the plate may include an anterior upward extension to fully occlude the passage running between the labial surface of the alveolus, alveolus, and nasal cavity. The plate may be constructed to include any congenitally missing teeth to improve articulation and appearance. Individuals who use palatal plates must be monitored periodically due to possible tissue irritation by the plate. Materials such as food particles, oral mucosalsecretions may cause buildup on the upper surface of the plate; therefore, it is essential to clean a palatal obturator at least twice a day to avoid tissue irritation.
Nance Obturator
This fixed obturator is based on the Nance appliance, which was originally used as a space maintainer in orthodontics, but has been redesigned for closing anterior palatal fistulas in patients with cleft lip and palate. The Nance obturator may be used when the surgical closure of the fistula is not feasible and a removable device is not successful.
Speech Prosthesis
Pharyngeal Bulb Obturator or SpeechProsthesis:This prosthesis is given in case of patients with velopharyngeal insufficiency where there is anatomic deficiency of soft palate so that it is unable to create positive seal with posterior and lateral pharyngeal wall. Pharyngeal bulb obturator has a palatal plate retained with the help of clasps and a posterior bulb replacing the deficient part of soft palate. This will provide hard and stable base against which posterior pharyngeal wall contracts to bring about velopharyngeal seal. It can be either interim speech aid prosthesis made of heatcure acrylic resin or definitive prosthesis involving cast partial denture framework.
Fabrication technique involves making of alginate impression of maxillary arch taking care to record as much posterior part of soft palate as possible. This is followed by fabrication of working cast and acrylic plate is adapted on the cast with posterior wire extension which reinforces speech bulb. Impression of pharyngeal portion of the prosthesis is done using impression compound. This is followed by functional impression of the tissues using mouth temperature waxes or tissue conditioner. These impression materials later will be replaced by heat cured acrylic resin.
Palatal Lift Prosthesis
Velopharyngeal incompetency is a clinical condition where soft palate is not anatomically deficient but functionally weak leading to inadequate contraction and inadequate contact with posterior pharyngeal wall. This leads to nasal resonance and reduced speech intelligibility. This condition may be due to poliomyelitis, muscular dystrophy or myotonia. Children with this condition can be rehabilitated with palatal lift prosthesis. Similar to pharyngeal bulb obturator it has two component oral and pharyngeal components. Pharyngeal part lifts the palate and approximates it close to the posterior pharyngeal wall so that positive velopharyngeal seal can be created.
Dental Implants In Pediatric Patients
1. Osseointegrated implants have been successfully used in dentistry for adults since the discovery of implants by Branemark in 1969. In adults, the success depends on the quality and quantity of bone and proper treatment plan, surgical technique and proper oral hygiene measures. These factors are also equally important in growing children but another critical factor that has to be considered is the ongoing growth and development in children and adolescents. Teeth loss due to trauma and congenitally missing teeth are often encountered in young children , so in such cases removable prosthesis, Maryland bridge or orthodontic movement of teeth to close space are usually the treatment modalities , because jaw growth is not completed. However, these options may lead to increased caries rate, increased residual alveolar resorption and other periodontal complications. Implants can be a good alternative because it can prevent residual alveolar resorption.
2. Other factorsthat favors early placement of implants in children would include excellent local blood supply, positive immunological resistance, uncomplicated osseous healing. When restoring the edentulous space in young children and adolescents using implants,the basic knowledge of growth and development is essential to assess the implants’ response to craniofacial growth. Implants behave like ankylotic teeth and fail to move together with the surrounding structures leading to infra-occlusion of implants and difficulties with prosthesis.[13].
A basic knowledge of facial growth is critical in assessing how an implant may respond in the adolescent. An osseointegrated implant behaves like an ankylosed primary tooth because both lack a periodontal ligament. The periodontal ligament has an important function in allowing teeth to erupt and adapting for dentoalveolar and facial growth, not only vertically but also in anteroposterior and transversedimensions. Early animal studies have shown that osseointegrated implants remain fixed in their initial position and cannot adapt for growth changes.[14]
Growth of the Jawbones
Growth is first completed in the transverse plane thenin sagittal plane and finally in vertical plane.[15] Thegrowth of mandible is closely associated with generalbody growth, whereas growth of the maxilla is moreassociated with the growth of the cranial structures.As a rule of thumb, which applies to both the maxillaand mandible, transverse growth is first completedbefore the pubertal growth spurt and is followed by growth in length and finally growth in height, which is completed last.[16]
Maxillary Growth and Implants
Transverse Growth
Growth in width of the median palatalsuture accelerates at puberty and is the most significantfactor in transverse growth of the maxilla. Implants placed in the central incisor region will result indiastema with the adjacent natural teeth and shift inthe midline.[17]
Sagittal Growth
The maxilla usually grows in a downward and forwarddirection relative to the anterior cranial base. Althoughthe initial growth is related to growth of cranialbase, the maxilla shows much greater changes fromage 4 to adulthood than does the cranial base.[18] Maxillary growth occurs as a result of both passivedisplacement and enlargement. During early childhood,passive growth is a major factor in a maxillary growthbut becomes less important as anterior sutures of thecranial base closes. After the age 7, approximatelyone-third of the maxillary growth is accounted forpassive displacement. The other two-third occurs as aresult of enlargement of maxilla itself.Resorption in anterior region will result in gradual lossof bone in the labial aspect of the implants resulting inlabial fenestration and exposure of implants.[19]
Vertical Growth
Vertical growth of the maxilla occurs by suturallowering i.e., passive displacement of maxilla andapposition on the tooth-borne surfaces of the maxillaryalveolus. The orbit enlarges with increasing eye size withcompensatory apposition at the floor of the orbits.[20],[21] Thenasal floor is lowered by resorption on its nasal surfaceand by deposition on the palatal and alveolar surface.Hence, as the alveolus increases in height by appositionon its occlusal aspect, it is simultaneously decreasedby resorption at the nasal floor. Approximatelyone-third of the total increase in alveolar height isaccounted by nasal resorption. Therefore, observationfrom dental casts reflects less than two-thirds of thetotal amount of vertical alveolar growth. Resorptivelowering of the nasal floor is strongly differentiatedand is usually greater anteriorly than posteriorly.[22] This differential pattern is a compensation for therotational displacement of the maxilla in whichthe posterior segments roll downwards at a greater ratethan the anterior segments. Vertical maxillary skeletalgrowth dramatically affects implants.To prevent the complication in the vertical growth dueto remodeling it is advisable to delay the placement ofimplant till 18 years or till growth is completed.
Mandibular Growth and Implants
The timing of mandibular growth is similar to that ofmaxilla but not identical. The differential growth ofmandible converts the convex profile of child into astraight profile in adults.[23]
Transverse Growth
Changes in the width of the mandible are much lessthan in the maxilla. The increase in the width of themandible occurs primarily in the posterior region ofthe mandible. As the mandible increases in length, italso increases in posterior width because of its V-shape.The width in the anterior mandible ceases due to earlyclosure of mandibular symphysis (around 1-year).Thus, mandibular anterior width stabilizes relativelyearly and increases only slightly by appositional growth,whereas mandibular posterior width increases with theincreasing length of the mandibular body.Implants can be placed in anterior mandibular regionat an early age. But implants in mandibular posteriorregion of growing children will result in lingual positiondue to bone remodeling in premolar molar region.[24]
Sagittal Growth
Changes in arch length in the mandible differ from thosein the maxilla. As the permanent incisors erupt, there isgenerally little or no change in mandibular arch length. Sagittal growth of mandible is due to both endochondralgrowth and remodeling of bone. The growth of thecondyle results in increase in the length of mandible.To accommodate posterior teeth, the body of themandible increases in length by resorption on anterioraspect of ramus and deposition on the posterior aspect.An implant placed in early age will result in exposureof an implant due to pattern of resorption.[25]
Vertical Growth
Mandibular growth increases by condylar growthand by bone apposition at dentoalveolar complex.When serial lateral cephalograms are superimposedon the cranial base, the mandible appears to growdownward and forward. Mandible does not necessarily grow downward andforward in a linear manner. Instead, the mandiblerolls forward, with apposition below the symphysisand resorption below the gonial angle. Thus, duringgrowth, the face and the mandible tend to rotate, withthe center of rotation influenced by the direction ofcondylar growth.[26]
Conclusion
It is not uncommon to find children with grossly carious primary teeth. In most of the cases, the only treatment possible is extraction of the decayed teeth, resulting in an increased number of children who require prosthetic rehabilitation with either partial or complete dentures.Most of the parents are negligent towards restorations and maintenance of primary teeth because of lack of knowledge about importance of primary teeth, reluctant to have prosthetic rehabilitation of their child at such an early age, economic constraints and lack of time to follow up with lengthy treatment procedure. Prosthetic rehabilitation at this stage is essential to restore masticatory function, appearance and muscle function; to maintain and improve phonetics; prevent development of deleterious oral habits; and to minimize possible psychological disturbances.
Prosthodontic rehabilitation of children with pronounced edentulismhelps to normalize the function of masticatory and perioral muscles, consequently the growth pattern of basal bones and gives psychological boost to the self – image of the child. Early rehabilitation of children will go a long way in helping them interact normally with their peers. But one must remember that any form of restoration or prosthesis should provide dentition confirming with the age of the patient.
References
1. Caldas AFJr, Marcenes W, Sheiham A. Reasons for tooth extraction in a Brazilian population. Int Dent J 2000;50:267-73.
2. Engle WA; American Academy of Pediatrics Committee on Fetus and Newborn, "Age Terminology During the Perinatal Period," Pediatrics, 2004, 114(5):1362-4.
3. Oginni FO. Tooth loss in a sub-urban Nigerian population: causes and pattern of mortality revisited. Int Dent J 2005;55:17-23.
4. Lee JK. Restoration of primary anterior teeth: review of the literature. Pediatr Dent. 2002 Sep-Oct; 24(5):506-10.
5. Pinkham JR, Casamassimo PS, McTigue DJ, Fields HW, Nowak AJ. Pediatric Dentistry: Infancy through Adolescence. 4th Ed. Philadelphia, PA. WB Saunders Company; 2005.
6. McDonald RE, Avery DR, Dean JA. Dentistry for the Child and Adolescent, 8th Ed. Mosby. 2004.
7. American Academy of Pediatric Dentistry. Pediatric Dentistry Reference Manual, vol. 31 (60), 40-46
8. Mathewson RJ, Primosch RE. Fundamentals of pediatric dentistry. Quint Pub Co Inc, Chicago, Berlin, London, Tokyo, Sao Paulo, Moscow, Prague, Warsaw, Third Ed, 1995, pp. 340-350.
9. AkshayB,Arun S, Sachet P and Renu B. Prosthodontic Management of a Child with Ectodermal Dysplasia: A Case Report. J Indian Prosthodont Soc. 2010 June; 10(2): 137–140.
10. . Mathew C A, Sudhakara V M, Karthik K S.The Sieved Resin Bonded Prosthesis. JIADS VOL -1 Issue 2 April - June,2010.
11. Kanazava T, Yoshida H, Furuya Y, et al: Sectional prosthesiswith hollow obturator portion made of thin silicone layer overresin frame. J Oral Rehabil 2000;27:760-764
12. Walter JD: Obturators for cleft palate and other speechappliances. Dent Update 2005;32:217-228, 220-222.
13. Sharma AB, Vargervik K. Using implants for growing child. J Calif Dent Assoc 2006;34(9):719-34
14. Thilander B, Odman J, GrondahlK, Lekholm U. Aspects of osseointegrated implants inserted in growing jaws. A biometric and radiographic study in the young pig. Eur J Orthod 1992;14(2):99-109.
15. Cronin RJ Jr, Oesterle LJ. Implant use in growing patients. Treatment planning oncerns. Dent Clin North Am 1998;42(1):1-34.
16. Percinoto C, Vieira AE, Barbieri CM, Melhado FL, Moreira KS. Use of dental implants in children: a literature review. Quintessence Int 2001;32(5):381-3.
17. Teixeira NC, Gurgel CV, Fernandes AP et al. Prosthetic rehabilitation in children: an alternative clinical technique.Case Rep Dent. 2013;2013:512951. doi: 10.1155/2013/512951. Epub 2013 Sep 24.
18. Bala S, Chugh A, Narwal A. Prosthetic Rehabilitation of a Child Suffering from Hypohidrotic Ectodermal Dysplasia with Complete Anodontia.Int J ClinPediatr Dent 2012;5(2):148-50.
19. Martin JW, Chambers MS, Lemon JC, Toth BB, Helfrick JF. Prosthodontic and surgical considerations for pediatric patients requiring maxillectomy.Pediatr Dent. 1995 Mar-Apr;17(2):116-21.
20. Bhargava A,Popli S,Bhargava R. Prosthodontic Management of a Child with Ectodermal Dysplasia: A Case Report. J Indian Prosthodont Soc. 2010; 10(2): 137–40.
21. Jain N, Wadkar, Nemane A, Katoch S, Dewangan A. Prosthodontic Rehabilitation of Hereditary Ectodermal Dysplasia in an 11-Year-Old Patient with Flexible Denture: A Case Report. Case Rep Dent. 2012;2012:489769.doi: 10.1155/2012/489769.
22. Artopoulou, Ioli-Ioanna; Martin, Jack W.; Suchko, George D.Prosthodontic Rehabilitation of a 10-year-old Ectodermal Dysplasia Patient Using Provisional Implants. Pediatric Dentistry. 2009;31:52-7.
23. Kumar P, Rastogi J, Jain C, Singh HP. Prosthodontic management of worn dentition inpediatric patient with complete overlay dentures:a case report. J AdvProsthodont 2012;4:239-42.
24. Bergendal B,Bergendal T,Hallonsten AL,Koch G. A Multidisciplinary approach to oral rehabilitation with osseointegrated implants in children and adolescents with multiple aplasia. European JournalOfOrthodontics 1996;18: 119-29.
25. "6;wider K,Szozda A, Tokarski T. Prosthodontic Treatment of Children – Cases Reports. Dent Med Probl 2013; 50:106–13.
26. Schneidman E, Wilson S, Spuller R. Complete Overlaydenturesforthepediatricpatient:casereports. Pediatric Dentistry 1988;10:222-25.
|
|
|
|
|
|
|